Saturday, December 04, 2010
Hey Arizona, ur doin' it 'rong...
Update (12-17-2010): still sounds like death panels to me. Wasn't this kind of thing supposed to happen under the watch of "liberals"? Never a state like AZ...
Tuesday, October 19, 2010
I was, am, and hope to always be naïve.

If I gave this image to a polite, random neuroscientist, he/she would give me a coy smile and say that the picture was “nice and the TUJ1 antibody stained very well.” If I gave this image to an impatient and nasty, random neuroscientist he/she would scowl at the piece of paper and ask me why I was wasting his/her time: I’m not showing anything new!
I hope this figure will be as stunning to me in a few years, when I’ve read more literature and seen more figures and done more research and graduated with a PhD. Sure I’ll see a lot of similar images; I might be bombarded by them. But I hope to appreciate that the ordinary is beautiful too: because you see it once, doesn’t mean the allure has to fade.
Monday, October 18, 2010
Monday afternoon football update
1. A Rutgers' University student athlete was paralyzed from the neck down after an in-game incident against Army.
Update (10-19-2010): The most recent medical literature says that 90% of patients with complete tetraplegia (aka quadraplegia) at one month post-injury remain complete tetraplegics for good. After 6 months, there is little change in a person's neurological status caudal to the spinal injury. In other words, the coming days and weeks will be hugely informative of the athlete's function long into the future. Here's hoping he regains function. Also, from what I have gleaned from the news reports, it does not appear that therapeutic hypothermia (TH) was tried. Recall that TH was used when Buffalo Bills' player Kevin Everett was injured back in 2007. Although the use of TH in his case is still being debated, he was able to walk within ~one month of the injury.
2. Yesterday's NFL games featured several instances of traumatic brain injuries.
Friday, October 08, 2010
walking, chewing gum
Sunday, October 03, 2010
Rethinking traumatic brain injury and its consequences: “repeated brain injury can change your life and your family’s life forever.”
“Mike Webster, the longtime Pittsburgh Steeler and one of the greatest players in N.F.L. history, ended his life a recluse, sleeping on the floor of the Pittsburgh Amtrak station. Another former Pittsburgh Steeler, Terry Long, drifted into chaos and killed himself four years ago by drinking antifreeze. Andre Waters, a former defensive back for the Philadelphia Eagles, sank into depression and pleaded with his girlfriend—“I need help, somebody help me”—before shooting himself in the head.”
Friday, September 24, 2010
Friday food for thought
Wednesday, September 22, 2010
It gets better
Tuesday, September 21, 2010
The creepy cashier and lessons in a heteronormative society
I waited in line at the grocery store as the middle-old aged clerk (65-70 years old) struck up this conversation with the young daughter (~6 years old) of a woman buying groceries ahead of me:
Girl: No. [giggles, looks away.]
Now, I laughed too. The clerk was just silly. The girl was predictable. The mother was amused. And I got to thinking, would people have reacted this way had the girl instead been a boy? What if the elder clerk was in fact a homosexual, and thus innocently struck up the same conversation with the woman's son. I doubt anyone (I included) would have acted the same way. People would say, "Oh, how dare he try to make her son GAY!" "God, he's such a creepy molester!" "What is he, a Catholic priest or something?" In other words, they are afraid of such behavior, because it might influence the boy. It might shatter his world view of boys + girls = love. Quite simply, when the heterosexual "norm" of our society is enforced, even by slightly creepy, but good-natured clerks, we all laugh and move on. Because we think that society is grooming everyone to be either gay or straight. Straight is ok. Gay? No homo.
I doubt it's so straightforward that society's influences play such a large role. If they did, we wouldn't have had people identify with homosexuality in the dark ages of sexual identity (pre-gay rights/civil rights movement, which is by the way ongoing: see the link above).
I hope my (future) children grow up in a world that embraces both the straight and the gay clerk. I have enough faith they will know how to figure out their own sexual identity, regardless of some old grocery store clerk's influence.
Wednesday, September 01, 2010
Kids and antipsychotics
I read bits and pieces of the “Diagnostic and Statistical Manual of Mental Disorders IV” (DSM-IV) during medical school, which was an informative yet frustrating experience: one that I would like to revisit and expand upon when DSM-V is released. My understanding of psychiatric illnesses and their diagnoses and treatments is extremely limited. I can only imagine how difficult it is to care for some psychiatric patients, let alone, children.
Enter Kyle. The NYTimes paints a grim portrait of his struggle with antipsychotic drugs:
“Kyle’s third birthday photo shows a pink-cheeked boy who had ballooned to 49 pounds.”
“Kyle smiles at the camera. He is sedated.”
“He was sedated, drooling and overweight…”
Kyle isn’t alone.
“Texas Medicaid data ... showed a record $96 million was spent last year on antipsychotic drugs for teenagers and children — including three unidentified infants who were given the drugs before their first birthdays.”
Kyle and other children from low-income families “were four times as likely as the privately insured to receive antipsychotic medicines” because it is “cheaper” than psychotherapy, according to a Rutgers U. study.
I wonder what things are like in the prison systems.
Wednesday, August 25, 2010
20-Somethings
In a way, doing extended post-college schooling may provide exactly what 20-somethings need: a transitional phase, gradually introducing more responsibility, life choices, and adult activities.
Who knows? As for me, I feel as though I identify much more with a "20-something" than a "young adult."
Wednesday, August 18, 2010
I know what I would want...
WTF is up with...
2. Building a Islamic community center (which includes a prayer center; by a subdivision of Islam which has NEVER been supportive of or involved in terrorism) two blocks from the former WTC site in lower Manhatten = "Ground Zero 9/11 Victory Mosque" ?
People babble over issues of which they have no understanding. And worse, they don't even try to understand. They just babble.
::sigh::
Tuesday, August 03, 2010
As you know end-of-life care is a big deal...
... that can improve quality of life for dying patients and save the government a lot of money. Chuck C has written about the so-called “death panels”; the NYTimes and other news outlets have expanded the dialogue; now Atul Gawande has written an essay for the New Yorker.
I’d like to focus on one particular part of Gawande’s essay, where he refers to Stephen Jay Gould’s remarkable recovery from abdominal mesothelioma, which inspired Gould’s essay “The Median Isn’t the Message.”
Gould beat a normally lethal cancer. He is the exemplar patient that all physicians would like to have and treat. Gawande admits this sentiment himself:
I think of Gould and his essay every time I have a patient with a terminal illness. There is almost always a long tail of possibility, however thin. What’s wrong with looking for it? Nothing, it seems to me, unless it means we have failed to prepare for the outcome that’s vastly more probable. The trouble is that we’ve built our medical system and culture around the long tail. We’ve created a multitrillion-dollar edifice for dispensing the medical equivalent of lottery tickets—and have only the rudiments of a system to prepare patients for the near-certainty that those tickets will not win. Hope is not a plan, but hope is our plan.
The reality, as Gawande alludes to, is grim: optimistic hope in sexy, new treatments against diseases that we don’t completely understand. The grim reality, though, funds our futures as physician-scientists. A lot of basic research in a lot of different fields is needed to know which patients will benefit from which treatments. And some times the treatments will be palliative.
Gould studied patient-survival curves. He saw “himself surviving far out in that long tail.” But what does it mean to be in the “long tail”? People are hard at working doing this, particularly with breast and prostate cancer.
Monday, August 02, 2010
First day for first years
Wednesday, July 28, 2010
Monday, July 19, 2010
"The Advantage of Being Helpless"
Updated, 7/21/2010: Title changed from "The Advantage of Being Hapless" to "The Advantage of Being Helpless." At least I didn't make up a word like "refudiate."
Thursday, July 15, 2010
Preventative tests at no cost
New rules from the U.S. Government's Executive Branch that insurance companies will be required to cover all costs associated with basic preventative and diagnostic medical tests. Good news indeed. Will save the ~100k lives, as quoted in the article and will probably also lower costs. This, like many other things, is incremental, but it's another notch on the belt.
Wednesday, July 14, 2010
Challenges, frustrations
That is, if we're ready to learn.
Being ready is easier said than done.
Tuesday, July 13, 2010
Hospitals as efficient factories of healing
Wednesday, July 07, 2010
I’m glad I visited Arizona before July 29, 2010…
You’ve probably heard that the federal government is filing suit against the state of Arizona. This isn’t the first time federal authority has found the need to “pre-empt state law when the federal interest is dominant and where there already exists a system of federal regulations.” It happened in our great state of California after our great citizens passed Prop 187 in 1994. I’m trying to imagine institutions like UCLA delaying care “until the legal status of that person has been verified" or holding workshops (like the ones Arizona policemen are receiving right now) to generate suspicion. It’s mind-blowing, really.
“Concerning the Interview”
Mark Twain wrote an autobiography. But he requested a 100-year posthumous release. UC Berkley will soon publish his autobiography, along with many essays, including “Concerning the Interview.”
The interview is an important, whacky, at-times-stressful component of the MD-PhD application process. It is an opportunity for applicants to distinguish themselves (for better or worse) from a crowd of incredibly promising applicants. While Twain’s perspective as the interviewee is astronomically different than the prospective MD-PhD student’s perspective (try saying that ten times fast), his comments deserve some serious thought.
“The Interview was not a happy invention. It is perhaps the poorest of all ways of getting at what is in a man.”
Amen. On the interview day, schools like to lighten tone by saying, “Oh, the interview is a way for us to get to know you,” when in reality, the interview is an interaction that has been repeated over so many times (in past interviews or in front of the mirror or good friends) that it is essentially a rehearsed exercised: aka The Shpeel. I guess an interview is better than nothing. But I imagine there are moments when interviewees yield shadows of themselves in the wrong light (again for better or worse).
“You know by experience that there is no choice between these disasters. No matter which he puts in, you will see at a glance that it would have been better if he had put in the other: not that the other would have been better than this, but merely that it wouldn't have been this; and any change must be, and would be, an improvement, though in reality you know very well it wouldn't. I may not make myself clear: if that is so, then I have made myself clear--a thing which could not be done except by not making myself clear, since what I am trying to show is what you feel at such a time, not what you think--for you don't think; it is not an intellectual operation; it is only a going around in a confused circle with your head off. You only wish in a dumb way that you hadn't done it, though really you don't know which it is you wish you hadn't done, and moreover you don't care: that is not the point; you simply wish you hadn't done it, whichever it is; done what, is a matter of minor importance and hasn't anything to do with the case. You get at what I mean? You have felt that way?”
Give this some time. The first time I read it, I scratched my head. I’ve read it a few more times, and I’m not sure whether I really understand it. Perhaps that is the point (read: “it is not an intellectual operation”), and I’m empathizing with the experience, which I imagine is more generalizable, beyond the scope of just an interview. I personally found that the application process had me “going around in a confused circle with your head off,” especially when I thought too hard about questions that are unanswerable but unavoidable on ye-good-olde interview trail. The most blaring example was “Why MD-PhD?” I had answers to questions like this. They were tailored to fit my portfolio. But the deeper questions found ways to pop up. What did I do? Acknowledge them, and let them be. As if they were going anywhere. Hehe. And this abstraction segues into the last quotation that I will torture you with:
“Yes, you are afraid of the interviewer, and that is not an inspiration. You close your shell; you put yourself on your guard; you try to be colorless; you try to be crafty, and talk all around a matter without saying anything: and when you see it in print, it makes you sick to see how well you succeeded.”
(N.B. that I was not sick with success, unlike Mark Twain; but his zinger was too good to exclude.)
Now read the first quotation I provided. I’m not trying to be a Debbie Downer; I’m not trying to be jaded or pessimistic; but maybe these characteristics are seeping through my attempts at realism. And that reality also includes the many fun moments of the interview trail, like eating good food with the new friends and colleagues I met in the big or small city that I had never been to before. Ye-good-olde interview trail is an experience. “You get at what I mean?”
Monday, July 05, 2010
"If Homelessness Were Genetic"
Monday, June 28, 2010
The plot continues to thicken...
[Also, I'd be curious as to what the brains of other football (a.k.a. "soccer") players look like. "Headers" don't seem like benign meetings of the cranium and ball to me...something my mother worried mightily about when my sisters and I used to play organized soccer in our youth.]
Thursday, June 24, 2010
Alzheimer’s and the NYTimes revisited
Chuck C highlighted a NYTimes article about familial Alzheimer’s Disease (AD). Today I read a NYTimes article about the use of PET probes to identify AD.
Familial AD has guided current thinking re. the pathophysiology of AD: i.e. the role of amyloid plaques. The three genes implicated are amyloid precursor protein (APP) and presenilin 1 and 2. It is hypothesized that amyloid beta proteins (in particular aβ42) aggregate – and to make a long and complicated and continuously changing story short – cause inflammation and havoc that results in neuron loss. The cortical and subcortical neuron loss manifests as cognitive impairment and dementia, which are the basis for the clinical diagnosis.
Clinical diagnoses are imperfect. The push for markers is strong and lucrative. The NYTimes article that I mentioned earlier highlights the work of Daniel Skovronsky (who is an MD, PhD in industry) and the development of a F18 PET probe targeted against amyloid plaques. In short, the probe identified amyloid plaques that were confirmed in post-mortem autopsies. The work is a technical advancement over the prior C11 amyloid probe. I don’t know the probe’s sensitivity or specificity. And remember that the gold standard is a post-mortem autopsy staining for amyloid plaques.
Amyloid plaques may not be the whole story, though. Transgenic mice that express “abundant” amyloid plaques did not show a strong correlation with neuron loss, in particular the hippocampus. Individuals vaccinated against aβ42 cleared amyloid plaques, but the effects did not protect against neurodegeneration. Other hypothesized processes include i) hyper-phosphorylated tau mediating the formation of neurofibrillary tangles, ii) a decrease in acetylcholine synthesis, and iii) the loss of locus ceruleus neurons that synthesize norepinephrine. The complicated picture correlates with the current understanding of most AD cases, which are sporadic. Out of the many genes screened for associations with sporadic AD, APOE4 is the strongest risk factor. There are probably many more unknown protective and risk factors.
Skovronsky’s probe and other probes (including the ones tested here at UCLA) are baby steps in the right direction. Non-invasive, laboratory diagnostic tests are the holy grail of neurological and psychiatric diseases. And besides their diagnostic applications, in-vivo imagining has the potential to delineate amyloid and tau’s contributions toward the pathology and progression of AD. The NYTimes article states that “20 percent of people over 60 with normal memories had plaque”; these patients “were still statistically in the normal range,” and they “did worse on every memory test than the control group.” What does this mean? I smell longer studies.
But even more lucrative than diagnostic tests are pharmacological treatments. Acetylcholine esterase inhibitors (e.g. donepezil) and NMDA agonists (e.g. memantine) are symptomatic treatments only. I imagine pharmaceuticals have been salivating for some time… Meanwhile, the basic science must continue! Here is some bed-time reading.
Why Medicine?
Tough question to answer in 5300 characters or fewer. Not sure I ever wrote a good personal statement, or that I could in the future. Two years from now I will have to, for residency.
Something to look forward to.
And then there's always the wisdom of this guy, talking to graduates at Stanford recently. If you acknowledge that the practice of medicine needs to, and is, changing, maybe the field is for you. Or maybe it is not.
Wednesday, June 23, 2010
Tuesday, June 22, 2010
A health plan, 2 bucks a year
Monday, June 07, 2010
When the “Step One Adventure” (SOA) began...
... I considered posting updates, which sounded like a good idea, i.e. until I realized that most of my writing would be filled with angst and more angst. A little time has provided an emotional buffer, and I feel a somewhat comfortable providing commentary.
If you’ve taken SO, you know what I am talking about. If you plan on taking SO, you will soon. For everyone else, don’t worry: you aren’t missing out. Here are the cliff notes.
In a tiny little carrel on the eight floor of a building called “the Stacks,” I spent most of my day reading through “First Aid,” “BRS Pathology,” and “Rapid Review Pathology,” while doing USMLE World questions. Midway through my studying, I fled the stacks for my parent’s home. I drank better coffee, ate home-cooked meals, finished a first pass of the material, and started to make some headway on the Q-bank. When I returned to West LA, I avoided the stacks. My room became my cave. The days were spent hunched-over in front my computer, doing questions, questions, and more questions until I developed UWorld-burnout to go along with First-Aid-burnout. I tweak my back from poor posture; I developed a mild fungal infection on my left elbow. At this point my body hated me and I was ready to get the SOA over with.
There were times during the process when evil little thoughts tempted me to postpone my test date. “Anthony, you could do better if you had an extra week.” “Anthony, there is so much more high yield material to go over.” Now that I’ve taken the exam, I could not imagine the unnecessary suffering I would have put myself through. I accepted the gaps in my knowledge. And as Chuck C told me, I had to “trust the preparation.”
The preparation was both hellish and useful. The experience forced me to work really hard for a substantial amount of time. And while I worked hard, I tried harder to keep sight of the bigger picture: life will go on after the test. The SOA wasn’t fun, but there people out there who are having much less fun all the time. Let’s count our blessings, folks.
Wednesday, June 02, 2010
Alzheimer Disease - "earlyonset" and new therapies
Sunday, May 09, 2010
One year??!
I will have my PhD in one year's time, but do I really have the mind of a scientist? At this point, I can't help but think how woefully inept I am at planning, executing, analyzing, and proposing scientific studies. Though I've come leaps and bounds about how to think about science (so much of it seems like OBVIOUS common sense, so much else of it seems uncertain and difficult to grasp), I still feel as though I don't know shit. Maybe that means I actually am on the path, and that I've made much progress. Perhaps; time will tell.
Sunday, April 25, 2010
Failing trials...
To me, this issue is fairly complex and does not just simply boil down to the need for a "better managed and funded" system. It requires a fundamental change in the way drugs are developed, evaluated, and then applied to certain disease states.
Saturday, April 24, 2010
Treating the scars of war
Thursday, April 22, 2010
Posting slow-down
Saturday, April 17, 2010
Thursday, April 15, 2010
Change we can believe in
It warms me to see our President doing something about an issue that has tormented same-sex couples for as long as they and their partners have been faced with medical issues.
Regardless of how one feels personally about the issue, no one can deny that the patient possesses autonomy in who he or she designates to be the equivalent of "next of kin."
Because to not do this, we are systematically denying patients a fundamental right.
Wednesday, April 14, 2010
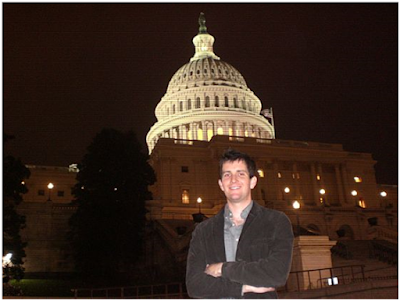
Photo at Capitol, 3-21-2010
Infections persist
Tuesday, April 13, 2010
A great NYTimes blog to check out
Agriculture report
On the flip side, there are about 1 billion under-nourished persons on the planet. With lower crop yields in areas particularly susceptible to the effects of climate change, that number promises to increase, perhaps by as much as 230% by 2050, without substantial increases in crop yields elsewhere in the world. Read this for more. (Subscription to Science may be required.)
Monday, April 12, 2010
H1N1 - it's all in the structures
This week's least surprising story
Sunday, April 11, 2010
The road ahead is well traveled
To celebrate the first two years of medical school, our class hosted a little shindig atop the hills of Westwood, with free booze and food and some speeches. The event was not bitter-sweet. I feel ready to move on. Perhaps the sentiment will change. Maybe not.
Don’t get me wrong: I’ve thoroughly enjoyed my two years in medical school. I could not have asked more from my peers and mentors. I’ve grown in a comfortable environment. While the curriculum was not perfect, it was good. If I had to enter my third year of medical school, I feel like I would be ready. I’m on my way to adult-like responsibilities that are real and serious. Strange.
I don’t know what to expect of graduate school. But I am mentally ready. I am mentally ready to finish the year strong with boards, a break, and research. I’ll take more classes and do more research. I’ll stop taking the classes and continue research until I’ve completed enough to resume MS3. The granular roadmap is in place. Now it is time to fill in the details.
I’m trying not to get ahead of myself. First things first: i.e. 1) study hard through finals and until boards, and 2) stay healthy by a) exercising, b) eating well, c) sleeping, and d) valuing my relationships.
The road ahead is well traveled with a lot of trails. A picture of my path is attached below.

Would you prescribe a hallucinogen...
The here, the now
There is no need to stew over who we might become, what we might do, and where we might go in the minutes, hours, days, weeks, months, and years ahead. What we have at the present is more than enough to sustain us. The moment in which we live is the most important one.
These are especially timely words, both for those who ponder their next steps -- all you re-visiters out there, persons in flux within their ongoing schooling (e.g. transition to PhD phase), and everyone else, wherever they find themselves -- and those of us attempting to extract meaning and peace in the present. It truly is all about the here, and the now. Life pulses along.
Thursday, April 08, 2010
That's what I'm talking about
Wednesday, April 07, 2010
Health Care Reform REDUX
*About one year ago, early in his first term in office, President Barack Obama laid out an ambitious goal: to have health care reform passed before the end of his first year in office.
*He wanted it to be hopey, changey, and bipartisany. Mistake number 1.
*So, in the Senate, a "Gang of Six" -- Max Baucus (Mont.), Jeff Bingaman (N.M.) and Kent Conrad (N.D.); and GOP Sens. Charles Grassley (Iowa), Mike Enzi (Wyo.) and Olympia Snowe (Maine) -- was assembled. The thought was that if bipartisan ideas went into the legislation (WHICH THEY DID), both parties would be able to vote for the bill. Mistake number 2.
*The "Gang" stalled and stalled, got nothing substantive done before the summer recess. Giant Mistake number 1.
*Media, special interests, opposed legislators, and any and all saboteurs-de-healthcare descended on the "Summer of Townhall Hell" where angry constituents admonished their democractically-leaning colleagues for hinting that they were supporting A) Death Panels, B) Health Care rationing, C) The Government interfering with Medicare, D) Mandatory and state-sponsored abortions, E) Defying the will of a minority of elected officials (Republicans), F) All of the above, and then some.
*With endless lies, spin, misinformation, and anger widely disseminated by the media, public support for health care legislation began to decline. Recognizing that bills are drafted, debated, voted upon, and passed by the legislature, the White House declined to intervene too much (per its role to sign bills into law and to enforce existing laws of the land). Constitutional role be damned, Giant Mistake number 2.
*Remarkably, despite death panels and major updates on health care reform from such renowned experts and Sarah Palin and Betsy McCaughey, by Christmas legislation had cleared both the House and the Senate. All that was left was for the two bills -- which had similar amounts of spending, deficit reduction, language on abortion, proposed changes to medicare; while differences on excise taxation of Cadillac union healthcare plans and kickbacks for equivocal moderate Democrats' participation -- to be merged in conference, filibuster prevented by 60-member cloture vote, and sent to the President's desk before long.
*Martha Coakley -- Attorney General of the State of Massachusetts -- managed to lose the special election for the Senate seat long held by Ted Kennedy. With Scott Brown, the Republicans had their 41st vote -- enough to successfully filibuster any and all changes to the Senate health care bill after conference committee between the House and Senate. Pundits of all shapes and sizes, party affiliations and persuasions, declared health care reform dead.
*Then, Democrats -- most notably Pres. Obama, who has a knack for coming back from behind (as an example, see this video of him dismantling Clark Kellogg in the presidential version of H-O-R-S-E, aka P-O-T-U-S), grew a pair and remembered how all parties in the majority have tended to use budget reconciliation as a way to bypass the often outdated/overstated/all-too-often-threated filibuster. So, despite objections to the contrary, they put "on the table" budget reconciliation. It came down to this: if the House could pass the Senate Bill verbatim along with another bill making changes to the Senate's bill, then the Senate could pass the changes using budget reconciliation. However, people wondered whether Mr. Obama could support this. He was still giving the impression that "all options were on the table."
*On 29 January, 2010, President Obama schooled the shit out of House Republicans. He showed that, unlike his noble objectors, he had thought through why reform needed to happen, and relatively all at once. He demonstrated that he had anticipated the kinds of questions he would be asked. And when conservative mouthpieces like Fox news cut away, while liberal mouthpieces like MSNBC are so happy it looks like they are scandalously satisfying themselves on air, you know something big has happened. And indeed it had. The rest of what happened was relatively predictable.
*More opposition and rabble-rabbling occurred. The "summit" at the Blair House produced no evidence of consensus or Republican support. And the President continued to look like the adult in the room. And he said, pretty unequivocally, that he was done playing games and he expected health care reform to pass.
*Then, Nancy Pelosi went to work, whipped up the votes over a period of about two months. A few hiccups here, a few there (such as the "deem and pass" almost-debacle which wasn't necessary because it wouldn't have changed anything anyway, but WSJ always seems not to care about the facts), and suddenly, it was down to "just" abortion (yay!) and with a little wrangling here and there an executive order would confirm what was already in the Senate bill to begin with.
*Late in the evening of 3/21/2010, the House passed the Senate Bill, along with some fixes. Two days later, this was signed into law. By the following week, all of the changes were, too, passed into law.
I will post my photo, in front of the Capitol, on 3/21/2010 as soon as I can find it.
The real work of fixing health care -- insurance, delivery, disparities, outcomes, disease management, coverage for everyone, and so on and so forth -- is what comes next. I intend to vigorously follow and post on how this can and will be accomplished.
Many tweaks will be needed, perfection is not a realistic goal, but doing nothing is certainly no option...
It shouldn't begin in the clinic, and that's all right
In a quest to meet these expectations, medical schools do everything to be "clinical" from the start: patient interactions begin on day one, medical history-taking is taught before any principles of cardiovascular or pulmonary physiology are explored, every opportunity is taken to emphasize the "clinical" relevance in all aspects of medical education, and small groups are formed ("Problem-Based Learning" [PBL]) to discuss "clinical" cases.
Must. Have. Clinical. Only. Always.
Relax, people.
Let's not kid ourselves. Simply discussing how a topic (say, for instance, the molecular development of a certain type of cancer) relates to a clinical diagnosis (say, a diagnosis of melanoma) does not mean that the curriculum is "clinical." It means it's putting basic scientific curriculum into the proper context. Contextual learning is not clinical learning, and nor should it be. If one were to start Day One of medical school learning the clinical aspects of melanoma, it would mean learning treatment algorithms, the principles of managing Il-2 patients, and the best practices for detecting and treating recurrent lesions. That approach of course wouldn't work if someone has no idea about skin physiology and anatomy, to say nothing of basic cancer biology.
My point is not to dismiss all clinical learning from the beginning. I think that the way in which doctoring/clinical skills are introduced in the first and second years of medical school are hugely beneficial. To be thinking about how a history is taken is a huge asset to how students learn the material.
To dismiss the first two years' physiology, anatomy, pathology, and so on -- in favor of watered down, "clinically-oriented" curriculum -- is to do a disservice both the medical students and the medical school as an institution. There is no substitute for having an understanding of the basic science of medicine. To whatever extent that material can be integrated with clinical examples is both instructive and beneficial. However, when it is replaced or challenged by students, faculty, and administrative powers-that-be with comments to the effect of "we want only the clinical 'high yield' info," core elements of the medical school experience are eliminated. And then everyone loses.
So please, let's refrain from obsessing over whether it's clinical and focus instead on whether the information is integrated, useful and necessary. I would bet all that "basic" science -- anatomy, physiology, histology, pathology, molecular biology -- is crucial to the education of the doctors of the future. The algorithms and protocols can wait. The basics need their place in education, too.
Tuesday, April 06, 2010
Saying "No"
This is the beginning of what I have claimed for a while. Health care reform needs to happen, and then we (as physicians, students, nurses, administrators, patients, families, and so on) need to be part of the change.
And it can be done.
Sunday, April 04, 2010
The struggle against dying
Wednesday, March 31, 2010
Bodies altered
Tuesday, March 23, 2010
"And yes Mr. Vice President, you're right... "
I will offer a long summary of the run-up to health care reform, but for the time being I am waiting to see whether the Senate will pass the "fixes" through reconciliation. Today, Senator Max Bacus (D-Montanta) suggested that perhaps not all the fixes would pass muster under the "Byrd Rule" which limits what falls under the category of "budgetary" changes [to avoid filibuster, changes to the original senate bill can be only budgetary in nature]. This would mean a potentially painful back-and-forth between the House and Senate. However, lots of things Bacus (and other Senators for that matter) have said to this point haven't turned out to be true. So who knows? Besides, the Senate bill (fury over "kickbacks" to poor people needing health coverage aside) is pretty damn good on its own. So I still think this is all good. But now is the time for the real work to begin.
Sunday, March 21, 2010
It is done...(now the Senate can finish)...
More thoughts to come (and my photos in front of the Capitol Rotunda).
This is a moment.
Now is the time for us all to take charge in making health care better in the United States. Thanks to the Congress, we now have a fighting chance.
Close!
Do it!
Thursday, March 18, 2010
the equinox
If yesterday and today and tomorrow are signs of what is to come – when spring is in full swing and the fever is full blown – then Yippee-ki-yay. Spring is going to be nice. Summer will be nice too. But winter wasn’t that bad. Sure we had some rain, some wind, and some cloudy days in LA. But let’s celebrate anyway: the good, the slow, and the non-idyllic times passed. Let’s take a moment and appreciate everything wonderful around us. This Saturday the earth and sun will dance, like they have been for more years than I count, and at 1:32 PM EDT they will pause to change hands. The sun’s leading the earth, but it takes more than one (us included!) to tango.
Friday, March 05, 2010
Exercise is good, mmmmkay
New Rule, ctd.
If there will be drastic cuts in education spending, then there should also be cuts in Medicare spending.
Fair is fair.
Wednesday, March 03, 2010
"Let's Get it Done"
Could this be the beginning of the end of the clusterf*&* of HCR, for now? We shall see.........
Friday, February 26, 2010
Molecularly-targeted therapies: hope, and challenges
Enough.
Health care reform looks to be in peril. Again. What's new?
As a future health care professional (resident, fellow, attending), I have taken an active role in writing, talking, and stewing over HCR debates currently going on in this country.
There has been an abundance of misinformation, grandstanding, and frustration. Many of us who are intimate stakeholders in this game -- who will provide the care in the future -- have wanted it to work. The non-medical professionals -- the citizens, the congresspeople, et al -- have framed the debate in their terms. They say reform, in its current manifestations, is unpopular. They say the American people want to start over. They say health care in America is the best in the world.
OK, let's try it. Let's keep things where they are.
But I have no sympathy for the people who start complaining about escalating costs, overcrowded emergency rooms, and denials of care. Does this sound callous? Absolutely. But enough is enough.
I'm trying to finish a PhD and get back to the wards. I'm trying to become a good doctor. And the whole public debate on health care reform is so pathetic, so "missing the point," so embroiled in death panels; and now, in today's news the opponents of reform (after all "we have the best health care in the world") are suddenly "noble" opponents [go to the New York Times, David Brooks column, examine Politico.com for analysis of the "tie goes to the GOP", and so on]. Look, people who think it's all good: if it's so good for you, then I'll see you in ten years. I'll treat you, but it's going to cost you.
Because everyone thinks it's hunky dory, cool. I will still have a job, I will still get paid, and you're going to pay. So let's all go in on this experiment. See how it works for you.
It's not going to be pretty.
Thursday, February 25, 2010
Oh hey blowhards in Congress
1. People arguing against health care reform, with the conclusion, We have the best health care system in the world. [No, we don't. We have probably the highest quality of care, in a number of top-notch health centers; it's the best health care when and if people can afford the care. Otherwise, we're disgracefully average among developing nations, for a SHITLOAD MORE OF THE COST.]
2. People arguing against health care reform, arguing it costs too much and will raise the deficit, who proceed to rail against cost-cutting measures in medicare, saying, But our seniors won't want their benefits slashed. It's partisan hack-ery; it's pandering; it's hypocritical; it implies that every dollar on medicare is a dollar well-spent.
3. Equally ignorant/partisan Democrats.
4. John McCain.
5. People who have good health care, with comprehensive coverage, who say that people who lack health insurance should start health savings accounts. If someone makes $20.00/hr, how much of that do you someone can set aside into a HSA? What if the person gets cancer? What about this person's children?
6. People who think medical malpractice reforms will magically cure health care of its ills. [No, it won't. States, like CA, who have adopted reforms, are seeing absurd increases in premiums.]
OH HEY LEGISLATORS: HEALTH CARE REFORM NEEDS TO HAPPEN, INCREMENTAL APPROACHES DON'T WORK. OH, AND YOU SUCK.
I have a new rule: no one in congress gets health care until the 30+ million people in this country without health care get it.
Great, problem solved.
Friday, February 12, 2010
Obesity shortens lifespan, BIG caveat
But, this study was done in Pima Indians, and the Pima have long been known to have a severe predisposition to diabetes and obesity (they frequently show up in medical textbooks as the prototype for a population susceptible to type 2 diabetes); and Native American populations throughout the US and North America have a number of other serious co-morbidities (low socioeconomic status, high substance abuse rates, etc) that could make this study difficult to generalize to the rest of the US population, which of course is highly heterogeneous.
So, this study - targeting a very small and genetically unique population in the US - should be taken with a sizable grain of salt.
Thursday, February 11, 2010
Questions, Answers
Research becomes exceptionally challenging when data can be filtered, distilled, treated, and then presented in such a diverse number of ways so as to obscure the initial question one was attempting to answer. At that point, finding an answer isn't really the problem. Understanding where the question is hiding is the challenge; searching is lonely work, in the sterile confines of a blanked mind...
Sunday, February 07, 2010
What?
Step 2: No one listens to you.
Step 3: Write letter to medical board.
Step 4: Get fired for blowing the whistle.
Step 5: Get indicted in state court for blowing the whistle.
I mean, say what you want about how things are in California, but really, Texas? That's shady. That there was good basis for complaining about what the physician did seems to be obvious (duh?) evidence against going after the whistle blower...But who knows.
Friday, February 05, 2010
FYI: blows to head cause problems
Wednesday, February 03, 2010
Finish the job, pass the damn bill
Monday, February 01, 2010
Concussions in youths
Sunday, January 24, 2010
Meanwhile, in the NFL
It's fascinating to see how sports leagues address the health of their players, particularly in football, where young men are part of one of the world's most finely-tuned and closely-watched experiments in traumatic injuries.
It's also a little grotesque.
Friday, January 22, 2010
The ranting will continue until morale improves
1) If you go to med school, you have decided you want to get into the health care "game." Therefore, you become a part of this "game" - you and it are linked. Like in avatar, you take your pony tail and fuse it with the health care dragon. You and it form a connection. To deny this is to not just be ignorant; it almost suggests nihilism - if you fail to care about what you do for the majority of your life, how can you say you really care about anything?
2) Empathy. Empathy. Empathy. The very best doctors all have empathy. And cultivating a sense of empathy is a lot harder than it seems. I think that, at the age of 26, I'm only beginning to think about how to live with a sense of empathy. It's perhaps the most important quality one can have. After all, we care for other human beings. That might sound cheesy, but it's the truth.
The imperative for HCR
And here, for me, is the moral argument. What has grated me the most during the HCR debacle is that the nihilists running Washington (I leave the president out of the nihilists camp, because I believe he actually gets the importance of HCR.) have some of the best and most expensive health care in the world. They say, "Let's take a breather, the American people are frustrated with how we are approaching this...Health care reform can wait." Yes, to those who have coverage, HCR can wait. Tomorrow, when a member of congress experiences chest pain - worried he might not be re-elected in the fall - he can go to a medical center of his choice and be worked up for a possible myocardial infarction (heart attack). When the barrage of medical bills arrive, the employer (we, the people, of whom 30 million plus lack any kind of insurance coverage) will pick up the tab. And so, the congressman returns to work, owing nothing for his care. A second job will not be necessary to pay for stenting the congressman's coronaries. Bankruptcy will not be necessary. The belt will not need tightening. In short, there will be no sacrifice required to treat the congressman's damaged heart. You see, I don't think lawmakers really understand what it's like to lack health insurance. I don't think they really get how bad it is, to be sitting in the emergency department or intensive care unit knowing that financial ruin looms. I don't think they get it. As a medical student, I have seen patients who don't have insurance, and their look is noticeably different from those blessed to have health insurance. They become consumed with trying to emerge from illness and bankruptcy. Just like you can spot homeless people in a crowd, you can spot uninsured patients in a hospital. The weight of their problems is palpable.
The Senate bill is far from perfect. But it's a vital first step. And I just don't think the privileged few who run Washington really get it. They seem totally devoid of empathy. I hope President Obama shows that he does and fights.
HCR experts: Senate bill far better than nothing
Thursday, January 21, 2010
Medicare coverage and outcomes
I'll try to post more on this, and other topics relating to how health care reform should and can happen, in future posts.
Wednesday, January 20, 2010
Health Care Reform: The Urgency of SOMETHING
As a stakeholder in the health care system - a future MD/PhD academic physician - I am deeply concerned about the current state of affairs in the system. The cost of delivering care is astronomical, with health care expenditures comprising ~16% of GDP, with no signs this number is going down anytime soon (by 2020, it will be close to ~20%). Despite the amount of treasure (personal, governmental) being devoted to health care, 15% of Americans have no health insurance. The largest government-run health insurance program - or more accurately, entitlement program - is Medicare. Estimates are that with no changes to the current system, Medicare will be insolvent by 2018. If future physicians think that this is no big deal, consider the fact that Medicare funds residency programs - it provides the salaries and other institutional support. So this is a big deal.
OK, those are some of the grim numbers. In short, we spend too much, we have no way to pay for health care if the status quo persists, and something must be done. Physicians don't wait for patients to go into multi-system organ failure (MSOF) before treating a patient with antibiotics, blood pressure support ("pressors"), ventilation assistance, and dialysis, etc, so why have we as a nation waited for the health care system to spiral into the shape it is currently in?
It's hard to say exactly why things have gotten so bad, and even more, it's hard to explain why the government has been so complacent. I think a big part of the problem is that bringing all of the players in the health care system - the doctors, the hospitals, the nurses, the technicians, the labor unions and employers who decide how to fund insurance policies, the insurance companies, the pharmaceutical companies, the diagnostic companies, the medical device manufacturers, the government, the patients, the lawyers - and having them agree on how to change the system and on which sacrifices they can accept is a massive (some think insurmountable) challenge. That is easier said than done, especially when said interest groups have varying degrees of influence ($) on Republican, Democratic, and Independent members of Congress.
I cannot say how exactly we should fix the economics of this broken system. I haven't looked at enough data, I don't understand all of the market forces at work, medical reimbursement practices; and I don't think most people in congress truly understand this either. And that's one of the first problems: the blowhards on both sides of the aisle in Washington use their opinions and empirical observations as a guide. Few (if any?) employ a rigorous treatment of the data. And that's the first place we need to start. As someone who has invested years of my life to learning how to design and execute good research, I think a first bold step would be to take the same hard look at medical care. That is, we need all of the pilot programs, evidence-based medicine approaches, properly placed incentives for good care, data sharing, electronic medical records, preventative measures - we need it all. These are the relatively cheap components of current proposals out there.
Whether - and how - to mandate insurance coverage for the whole citizenry of the United States is another question. The current proposals have done nothing to significantly change the costs of delivering care with respect to a mandate. They simply say that people should have coverage, the government will help if financially people have problems, and once covered, it's business as usual. So that's really not a good aspect of the current legislations.
Here's my take on health care reform: First, I want the death panels! So-called death panels - rather, having medicare reimburse physicians for having the difficult "goals of care" or "end of life" discussions is actually one of the best ideas that has been floated around, and it's one of the most politically polarizing elements of the reform legislation. And yet, it's one of the best damn ideas out there. Think about it: the bulk of medical care costs in a lifetime are incurred in the final months of a patient's life. Do a degree, this is unavoidable: if you get cancer and there's a chance to be cured, you'll try to treat it. But what if there is "no hope"? Or, more elegantly put, what if the realistic goals of care are palliative rather than curative? At that point, costs can be reduced dramatically (consider some of the data: http://www.reuters.com/article/idUSN06415881). But what's interesting is that when interventions are halted, usually suffering diminishes. The problem is that, all too often, doctors, hospitals, and providers in general either don't want to, don't know how to, or are financially incentivized not to have discussions about drawing down care and bringing people home. And so, more drugs are delivered, more treatments performed, more suffering ensues, all because who really wants to pull the plug on grandma? And sadly, most of the time, no one bothers to ask grandma what she thinks! And when they deem it time to ask grandma, she's already drugged up on sedatives/anti-anxiety/anti-psychotic drugs, in a hopeless ICU-induced delirium. At that point, few family members would be willing (and fairly so) to make executive decisions about where to go with care. Wouldn't it make good sense for patients - starting at a young age - to periodically have discussions with their doctors about end of life goals? Doctors ask whether patients sleep with men, women, or both; they ask whether it's cocaine, marijuana, heroin, meth, and/or all of the above; they ask about booze; they ask about depression; they ask about aches, pains; they ask about what concerns us the most. Why aren't they paid to have discussions about dying. After all, it's the one thing that will happen to every patient. And yet, this is the kind of stuff that has been maligned by opponents of health care reform legislation.
I want the pilot programs. The same kinds of government-funded and maintained programs that helped the agricultural industry in the U.S. become modernized could benefit health care immensely. And some of the privately- or state-funded programs already in existence prove this can work. Atul Gawande talks at length about this in a recent New Yorker piece. Note that he spends little, if any, time talking about public options versus mandates versus deals with pharmaceutical companies. He's talking about fundamentally changing how health care is delivered in the United States by empowering doctors and hospitals to make changes that benefit themselves, their patients, and the nation's finances as a whole. It will not happen overnight, but it can transform health care.
To make health care a truly sustainable and cost-controlled industry in the country will require more than just giving more people coverage in the same broken system. It will require innovative and progressive approaches to delivering care in the years to come. As examples, end of life discussions, in addition to numerous pilot programs embedded within current proposed legislation, offer some (of many) compelling ways to cut costs and do something rather than nothing when it comes to health care in the United States.
Stakes is high.